The Coronavirus pandemic has already had a devastating impact on the scuba diving world – but there’s another question on divers’ minds: ‘What happens if I get it? Can I dive after COVID-19?’ And the answer is not straightforward.
An article published in the German magazine Wetnotes (click here for a Google Translated English version) on 15 April gives an insight into the medical problems that scuba divers who have contracted SARS-CoV-2 might face. In it, Dr Frank Hartig, a senior consultant and response crisis coordinator/disaster officer for SARS-CoV-2 at Innsbruck University Hospital in Austria – and a scuba diver himself – describes some of the problems he has already encountered as a physician.
The acronym SARS – as in SARS-CoV-2, the official name of COVID-19 – stands for Severe Acute Respiratory Syndrome. SARS attacks the lungs, and while research into the long-term effects of the novel coronavirus is only just beginning, its physical impacts are all too tragically well known. Lung damage caused by conditions such as pneumonia and acute respiratory distress syndrome (ARDS) has been widely reported. It is also known to attack other organs, including the heart, although cardiac damage may go unnoticed until the heart is actually checked. Although we might not know much about the coronavirus itself, it has long been established that scuba diving with a compromised cardiopulmonary system can lead to serious injury, even death.
In his article, Dr Hartig describes his involvement with six active scuba divers who were hospitalised with conditions brought on by SARS-CoV-2 and who subsequently recovered and were discharged. When they returned for a check-up several weeks later, they all outwardly appeared to be healthy, but a closer examination proved otherwise.
‘The first checks of these six divers, who came to the check-up clinically healthy after 5 to 6 weeks, are interesting,’ writes Dr Hartig (translated from German). ‘In two of them, we saw significant oxygen deficiency when under stress as a typical sign of a persistent pulmonary shunt. In two others, bronchial tubes were still very irritable during exercise, as in asthmatics. Four of the six divers in the check-up CT [scan] still had significant lung changes. None of the six divers can be released for diving for the time being, despite their wellbeing.’
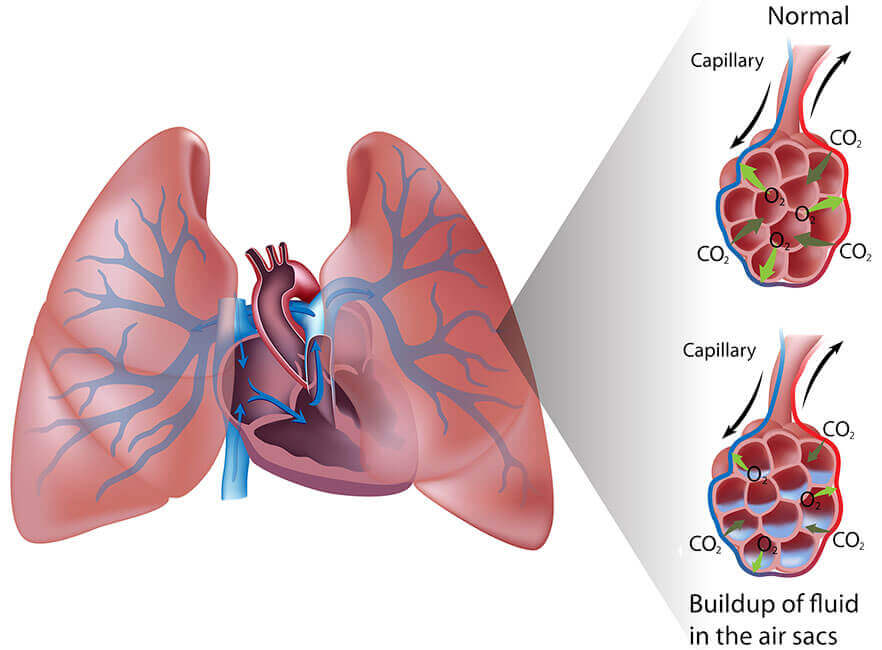
Exercise-induced asthma is a well-known contraindication to diving, and in layman’s terms, a pulmonary shunt is when blood fails to pick up more oxygen as it passes through the lungs, which leads to the body being starved of oxygen. It is often caused by fluid in the lungs, also the result of pneumonia and pulmonary oedema, a condition becoming widely recognised as a leading cause of diver fatalities.
At this stage, any questions over long-term damage to the lungs caused by SARS-CoV-2 would be entirely speculative, but it is clear from Dr Hartig’s assessment that divers who have been affected by the coronavirus should not dive until they have had a thorough medical examination – even if they otherwise appear healthy. As Dr Hartig notes, if proper precautions are not taken, ‘Young, COVID-healthy people who want to dive again quickly and appear healthy at first could [slip through our fingers].’
A report published on 12 April by the Belgian Society for Diving and Hyperbaric Medicine gives advice to scuba divers who may have contracted and recovered from Covid-19 based on current medical knowledge. To summarise, the report states that:
- Risk of Infection: Someone who has been infected with COVID-19 can still spread the virus to others. In a diving context that would be especially likely when conducting air sharing or rescue training exercises. Before returning to diving, divers should, therefore:
- Wait a minimum of two, preferably three months, if they had symptoms of the virus
- Wait a minimum of one month if they tested positive for the virus but were asymptomatic.
- Those who have not been tested and never had symptoms may still be susceptible to infection and should ‘observe a waiting period’ after lockdowns are lifted, which may be variable depending on location and type of diving.
- Divers and dive centres should strictly observe guidelines for gear disinfection as distributed by DAN
- Risk of Pulmonary Barotrauma: People who have had COVID-19 may have significant damage to their lungs for an unknown period of time, possibly permanently, and therefore have an increased risk of pulmonary barotrauma – or lung overexpansion injury – even if they don’t make rapid, breath-holding ascents. A diver who was hospitalised with lung-related problems should wait at least three months and undergo complete pulmonary function testing and a high-resolution CT scan of the lungs before returning to diving. Divers who had lung-related symptoms but were not hospitalised are still strongly recommended to have the test.
- Risk of Cardiac Events: Damage to the heart caused by COVID-19 may go unnoticed during the acute phase of the disease, but may lead to heart failure during diving. Therefore, it is recommended that a diver who was hospitalised with cardiac or pulmonary symptoms should, after the three-month waiting period, undergo a thorough cardiac evaluation with echocardiography and exercise testing (exercise electrocardiography – sometimes called the ‘stress test’). Those who had symptoms but were not hospitalised are strongly advised to have the tests as well.
- Pulmonary oxygen toxicity: It appears that some COVID-19 patients’ symptoms worsened after being given pure oxygen. Although little is known about an increased pulmonary sensitivity to oxygen, the report suggests it would be ‘prudent’ to avoid technical diving involving the prolonged breathing of hyperoxic gas with a pO2 of 1.3 ATA or higher. Simple nitrox diving (maximum pO2 of 1.4 ATA) should not present any problem.
- Decompression illness: tiny bubbles of inert gas form even on normal dives and are safely eliminated through the lungs during breathing. However, damage to the lungs may prevent the lungs’ ‘bubble filter’ from working and lead to an arterial gas embolism or other form of decompression illness. Ddivers who have suffered from pulmonary symptoms of COVID-19 should, therefore, remain well within the no-decompression limits of their dives.
Click here for the full report (available in French, Dutch and English)
A complete assessment of the problems that divers might face following a COVID-19 / SARS-CoV-2 infection is undoubtedly many months away and, as Dr Hartig notes, any long-term medical advice will remain speculative until clinical trials have been conducted.
In the short-term, however, the advice is clear. SARS-CoV-2 can damage the lungs and the heart. Scuba diving with damage to any part of the cardiovascular system can lead to serious injury and death. Much as we might all wish to rush back into the water as soon as we can, doing so without proper medical consideration may cause more harm than good.


